Is Anatomy Finished? | A Review of New Discoveries
TAPP Radio Episode 105
Episode
Episode | Quick Take
Are there really no more discoveries in human anatomy? In this episode, I’ll review some recent discoveries: the rise of the fabella, macrophage barriers, the interstitium, button and zipper junctions, lymph node micro-organs, new vessels in bones, and tubarial salivary glands.
- 00:00 | Introduction
- 00:41 | Is Anatomy Finished?
- 03:44 | Sponsored by AAA
- 04:16 | Rise of the Fabella
- 11:52 | Sponsored by HAPI
- 12:38 | Macrophage Barriers
- 23:18 | Sponsored by HAPS
- 23:55 | Interstitium
- 27:48 | Button and Zipper Junctions
- 35:28 | Lymphatic Micro-Organ
- 40:05 | Free Update Newsletter
- 41:05 | New Vessels in Bones
- 44:44 | Tubarial Salivary Glands
- 52:37 | Staying Connected
Episode | Listen Now
Episode | Show Notes
It is not over, unless you stop trying. (Nabil N. Jamal)
Is Anatomy Finished?
3 minutes
It’s easy to fall into that mindset that anatomy is “finished”—that there are no new discoveries to be made in the structure of the human body. But that’s simply not the case. In this episode, Kevin reviews seven anatomical discoveries discussed in the last few years of this podcast.
Sponsored by AAA
0.5 minutes
A searchable transcript for this episode, as well as the captioned audiogram of this episode, are sponsored by the American Association for Anatomy (AAA) at anatomy.org.
Don’t forget—HAPS members get a deep discount on AAA membership!
Rise of the Fabella
7.5 minutes
The fabella (pl., fabellae) is a small, beanlike bone that may (or not) occur behind the knee joint. Recent evidence shows that it’s showing up more frequently in the population. Why?
- The original version of this segment aired in Anatomic Variations in Humans | Fabella | Situs Inversus | Episode 43
- Fabella prevalence rate increases over 150 years, and rates of other sesamoid bones remain constant: a systematic review (recent research article) my-ap.us/2WkRSMs
- Sore knee? Maybe you have a fabella (plain English report from the BBC) my-ap.us/2Wmd6cN
- Fabella x-radiograph (to use in your course) my-ap.us/2Wm6Di3
- An illustration you can download as a PDF and use is available in the free TAPP APP theAPprofessor.org/TAPPapp
- Improbable Destinies: Fate, Chance, and the Future of Evolution by Jonathan B. Losos (book on updated ideas of evolution)
- amzn.to/2L9fzCE
- Browse The A&P Professor Book Club

Fabella image: Jmarchn (my-ap.us/2Wm6Di3)
Sponsored by HAPI Online Graduate Program
0.5 minute
The Master of Science in Human Anatomy & Physiology Instruction—the MS-HAPI—is a graduate program for A&P teachers, especially for those who already have a graduate/professional degree. A combination of science courses (enough to qualify you to teach at the college level) and courses in contemporary instructional practice, this program helps you be your best in both on-campus and remote teaching. Kevin Patton is a faculty member in this program at Northeast College of Health Sciences. Check it out!
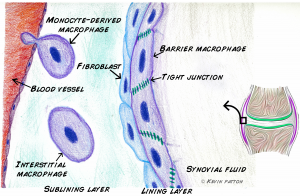
Barrier Macrophages
10.5 minutes
We knew there were macrophages within, and upon, the synovial membrane that lines synovial joints. What we have just learned is that macrophages on the synovial membrane surface can bind with tight junctions to form a barrier layer. Go figure.
- The original version of this segment aired in More on Spelling, Case, & Grammar | Episode 56
- Macrophages form a protective cellular barrier in joints (news summary) my-ap.us/33KVuLm
- Locally renewing resident synovial macrophages provide a protective barrier for the joint (research article) my-ap.us/33H5e9H
Sponsored by HAPS
0.5 minute
The Human Anatomy & Physiology Society (HAPS) is a sponsor of this podcast. You can help appreciate their support by clicking the link below and checking out the many resources and benefits found there. Watch for virtual town hall meetings and upcoming regional meetings!
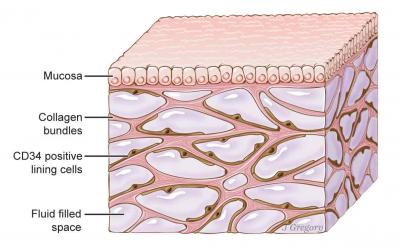
Interstitium
3.5 minutes
Has a new human organ discovered? Or is this news mostly hype? Or is the answer somewhere in the middle?
- The original version of this segment first aired in Test Debriefing Boosts Student Learning | Episode 11
- Structure and Distribution of an Unrecognized Interstitium in Human Tissues (original research report)
- Newly-discovered human organ may help explain how cancer spreads (article about the original report)
- That “New Organ” Everyone Is Freaking Out About Is Probably Not New (article outlining criticism of the original report)
- Is the Interstitium Really a New Organ? (another article interprets the original report)
- Is This Tissue a New Organ? Maybe. A Conduit for Cancer? It Seems Likely. (yet another opinion)
- The Human Organ Discovered in 2018 (and we have another opinion)
Interstitium. Illustration by Jill Gregory. Printed with permission from Mount Sinai Health System, licensed under CC-BY-ND.
Button and Zipper Junctions
7.5 minutes
Are you familiar with the button junctions that connect overlapping endothelial cells in lymphatic capillaries in a way that forms valves? What about zippers? Where do they fit into the story? (They do.) Here are some links to the details behind a great demo that Kevin shares for understanding lymphatic structure and function.
- The original version of this segment aired in Promoting Academic Integrity in Our Course | Episode 25
- Functionally specialized junctions between endothelial cells of lymphatic vessels (2007 research article outlining button and zipper junctions; great images)
- Plasticity of button-like junctions in the endothelium of airway lymphatics in development and inflammation. (2012 research article shows that zippers predominate in early development, but are then convert to buttons; also has some really cool images showing these junctions)
- Lacteal junction zippering protects against diet-induced obesity (2018 research article)
- Tighter lymphatic junctions prevent obesity (perspective and summary of the research article; includes a nice slide you can use in teaching)
Lymphatic Micro-Organ
4.5 minutes
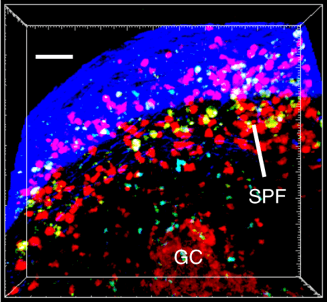
One headline announced the discovering of a new human micro-organ. It turns out, researchers have found a distinct structure just beneath the capsule of lymph nodes called the subcapsular proliferative focus (SPF) where memory B cells hang out—not deep in the germinal center (GC). This puts them in a good position to be activated by macrophages acting as antigen-presenting cells (APCs) and mount a strong secondary immune response.
- The original version of this segment first aired in Modeling Professional Integrity | Episode 26
- Researchers Discover New ‘Micro-Organ’ in Human Immune System (news item about the discovery)
- Memory B cells are reactivated in subcapsular proliferative foci of lymph nodes (research article from Nature Communications)
- Second Harmonic Generation Imaging Microscopy: Applications to Diseases Diagnostics (describes the SHG method used to visualize the lymph node cells; see image)
Free Update Newsletter from The A&P Professor
1 minute
A newly envisioned, newly styled, digital newsletter from The A&P Professor features news stories and updates in human science and education curated by Kevin Patton. To get your copy 2-3 times each week—or to simply check out previous editions—of this free newsletter, go to theAPprofessor.org/updates
[revue_subscribe]
New Vessels in Bone
3.5 minutes
Scientists have discovered a system of small vessels that cross every part of a bone’s cortical layers to supply most of the bone’s blood—over 80% of the arterial supply and 59% of venous drainage. The proposed name is trans-cortical vessels (TCVs).
- The original version of this segment aired in Big Year in Anatomy & Physiology Teaching with The A&P Professor | Episode 36
- We’ve discovered a new type of blood vessel in our bones (brief article summarizing the discovery) my-ap.us/2B6tHce
- A network of trans-cortical capillaries as mainstay for blood circulation in long bones (full research article) my-ap.us/2B6ttSq
- Video (gif) showing a virtual trip through a TCV my-ap.us/2B6XX6H
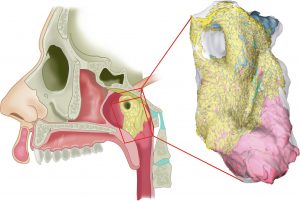
Tubarial Salivary Glands
8 minutes
A recent paper proposes the existence of a new organ—the paired tubarial salivary gland. It’s suggested that this be added as a major salivary gland along with the parotid, submandibular, and submaxillary salivary glands.
- The original version of this segment aired in New Organ | Dam Protons | Our Secret Language | TAPP 80
- The tubarial salivary glands: A potential new organ at risk for radiotherapy (original research article) my-ap.us/3khGFZe
- Doctors May Have Found Secretive New Organs in the Center of Your Head (newspaper article) my-ap.us/31L4RvV
- Cancer researchers discover new salivary gland (press release about discovery) my-ap.us/3m9mc9w
- Image: my-ap.us/3jgsO3T (CC license)
Need help accessing resources locked behind a paywall?
Check out this advice from Episode 32 to get what you need!
Episode | Captioned Audiogram
Episode | Transcript
The A&P Professor podcast (TAPP radio) episodes are made for listening, not reading. This transcript is provided for your convenience, but hey, it’s just not possible to capture the emphasis and dramatic delivery of the audio version. Or the cool theme music. Or laughs and snorts. And because it’s generated by a combo of machine and human transcription, it may not be exactly right. So I strongly recommend listening by clicking the audio player provided.
 This searchable transcript is supported by the
This searchable transcript is supported by the
American Association for Anatomy.
I'm a member—maybe you should be one, too!
Introduction
Kevin Patton (00:01):
The author Nabil N. Jamal once wrote, “It is not over, unless you stop trying.”
Aileen (00:10):
Welcome to The A&P Professor, a few minutes to focus on teaching human anatomy and physiology with a veteran educator and teaching mentor, your host, Kevin Patton.
Kevin Patton (00:25):
Is there really nothing new to discover in human anatomy? In this episode, I’ll review some recent finds.
Is Anatomy Finished?
Kevin Patton (00:36):
I have a question for you. Is anatomy finished? What I mean by that is have we discovered all of the structures of the human body, already mapped them all out? Well, of course not. There’s still a lot left to be discovered in anatomy. Not sure it’s true. We’re not going to find another organ the size of the liver or the size of the heart or the spleen. Probably. Who knows? Maybe we will.
Kevin Patton (01:14):
But it seems obvious that we’re not going to do that. But there may be something that size or maybe even just a little bit smaller, maybe some part of the liver or some part of the heart, that even at the macroscopic level we’ve seen before, might even have a name.
Kevin Patton (01:32):
But now we realize that, well, part of this is separate from the other part, structurally. That is, they have different structural characteristics and therefore probably different functions because we know that structure and function are intertwined with one another. So, we make those kinds of discoveries fairly frequently in anatomy.
Kevin Patton (01:54):
That’s true they may not be as frequent as in physiology. I don’t know that that’s true. But I’m just thinking it. That’s my impression. But I’ve heard this a few times recently, this idea that anatomy is finished. And haven’t you? Haven’t you even thought those thoughts? Maybe not. But I have. I don’t know if I’ve ever said it out loud. But I’ve heard other people say it out loud.
Kevin Patton (02:18):
And I know I’ve thought those thoughts that compared to physiology, anatomy is done. I mean, once you learn your anatomy, you’ve learned your anatomy. But of course, another part of me says, “No, that can’t be true because we are making new discoveries.” And how do I know that? …
Well, because I listen to this podcast. And also, I do the research behind each of the segments of this podcast.
Kevin Patton (02:45):
And over the past four years that we’ve been doing this podcast, there are a number of anatomy discoveries that I’ve talked about, that I’ve brought to you. And so, I thought, wouldn’t it be fun to go back and pick out a handful of those and review them? I wanted to do it just for my own purposes because I know that when I go back and review things like that, I understand them more deeply the second or third time around.
Kevin Patton (03:11):
And that certainly happened as I put together this episode because what I did was I took seven segments from previous episodes about anatomy discoveries, recent anatomy, discoveries. And I’ve taken those classic segments and I’ve put them into this episode. So, the whole rest of the episode is one segment after another, one discovery after another that you may have heard before in a previous episode but now it’s time to review.
Kevin Patton (03:39):
So, hey, let’s get going.
Sponsored by AAA
Kevin Patton (03:44):
A searchable transcript and a captioned audiogram of this episode are funded by AAA, the American Association for Anatomy. One of my favorite resources from AAA is their journal for teaching and learning anatomy and physiology. It’s called Anatomical Sciences Education. You need to check it out. And you can do that at anatomy.org.
Rise of the Fabella
Kevin Patton (04:16):
Here’s one of those structures that some folks have and some don’t, the fabella. It’s a bone but it’s not among the 206 human bones that we usually count as the standard bones of the human skeleton. So let’s take a quick look at what it is and where it is. Then I want to share some recent news about this interesting little bone.
Kevin Patton (04:41):
The fabella has that name because it resembles a little bean. A bean is faba in Latin and the ella suffix means little, so little bean. It’s a sesamoid bone. And we know that sesamoid bones are usually little bones that may or may not develop in the tendons or muscles.
Kevin Patton (05:02):
The only sesamoid bone that’s among the standard 206 bones that we count in the human skeleton is the patella of each lower limb. Most sesamoid bones are much smaller than the patella. And they may be present or not which is why they’re not common in the standard 206 bones.
Kevin Patton (05:25):
So here’s a good example of human anatomical variation. Variation from what? Well, from an arbitrary, perhaps even mythical ideal of a typical human. Really, it’s all about numbers. And I’m not sure any one person can identify themselves as “normal” or “typical.” But a lot of us are pretty darn close. And anyway, we have to start somewhere in our understanding of anatomy. So why not start smack-dab in the middle of a spectrum of variation.
Kevin Patton (06:01):
Sesamoid bones are called that because many of them are tiny little bones that resemble sesame seeds. These form in the tendons or muscles and could have any of several functions, like helping reduce friction within the tendon, helping redirect the force of muscle contraction, may be helping leverage the mechanical force of muscles like what happens in a patella or kneecap. Or sesamoid bones may just show up and have no function at all. Or worse, they could cause pain or get in the way of normal function.
Kevin Patton (06:40):
So, getting back to the fabella, this sesamoid bone sometimes develops in the tendon of the lateral head of the gastrocnemius muscle, just posterior to the lateral condyle of the femur. Some biologists think the fabella can act like a kneecap helping increase mechanical for some muscles. At least in some primates, that’s what happens.
Kevin Patton (07:04):
There are certain Old World monkeys that do this, but perhaps also including our pre-human ancestors. But we lost it along the way of evolution with it showing up only rarely now and again as a sort of extra little bone like the others that may show up in some individuals. But some recent news has some folks thinking that maybe the fabella is making an evolutionary comeback. That’s because it has become three times more common than just 100 years ago, jumping from all about 11% of the population having one or two fabellae to up to 39% occurrence in the human population.
Kevin Patton (07:54):
So, 11% to 39%, that’s a significant jump. I know some of us may be thinking, “Can evolution really happen that fast? A hundred years?” Well, if you’re thinking that, you didn’t read that book on evolution that I recommended you read in The A&P Professor Book Club a few months ago. It’s called Improbable Destinies. And it’s written by my friend, Jonathan Losos. Well, it’s not too late. You can still read it.
Kevin Patton (08:24):
And when you do, you’ll be amazed at how quickly vertebrate populations can shift their anatomy through evolutionary processes. Well, believe it or not, the fabella is showing up more often in humans. Now, you may ask why? What’s it doing for us? And why do we need it now? Need it now, get it? Need? It’s in our knee.
Kevin Patton (08:50):
Okay. So, I’ve resorted to puns because I don’t have a good answer to that question of why it’s happening. We’re not sure what it does for us if it does anything at all. But the team that discovered this increase in the incidence of fabellae speculated that may be a shift in nutrition over the last 100 years that caused the human skeleton to get larger and heavier could be putting the components of the knee joint under more pressure. And that’s what’s triggering the formation of a fabella.
Kevin Patton (09:28):
They also found out that if you have osteoarthritis, you’re more likely to have a fabella. But we don’t know if there’s really any cause-and-effect relationship with that. We just see it happening. So, that may or may not be part of the story. As a matter of fact, there are now just a lot of questions that need to be answered, but interesting and fun questions about human anatomic variation. I love science.
Kevin Patton (09:56):
By the way, before we leave this topic and go on to our next puzzler in the realm of anatomic variation, I want to mention something that this story reminds me of, a very strange phenomenon in the world of human anatomy and physiology teaching. Whenever the idea of keeping up with new and updated science content in A&P teaching and in the resources we use for teaching such as textbooks, I often hear something to the effect of that, “Yeah, physiology probably changes a lot over the years. But anatomy, anatomy doesn’t change.”
Kevin Patton (10:36):
Well, I hear this from students but I also hear it from A&P teachers. Now, I don’t usually agree with folks when they say this to me. But not being a fan of needless contradiction in conversation, I usually do just soft pedal my respond by not actually challenging them. But look here, we have yet another case of human anatomy changing over time, the evolution of human anatomy.
Kevin Patton (11:07):
Of course, that’s not something we see a lot of. But we sure do see a lot of change in our understanding of human anatomy, don’t we? As more specimens are studied, as more and different questions are asked, as old ideas are challenged, as our technology improves and we’re better able to observe, measure and explore the structures of the human body, our understanding of human anatomy changes a lot.
Kevin Patton (11:34):
In my opinion, I think we’re better educators if we don’t close the door on updates in human anatomy. I think we’re going to miss some very important ideas if we do that. Just a thought.
Sponsored by HAPI
Kevin Patton (11:52):
The free distribution of this podcast is sponsored by the Master of Science in Human Anatomy and Physiology Instruction, the HAPI degree. I’ve been on the faculty of this program at Northeastern College of Health Sciences from the beginning, just over 10 years ago. And I’m still excited about all the evidence-based teaching strategies that our learners apply directly to all the major topics in the typical anatomy and physiology course. Check out this online graduate program at northeastcollege.edu/hapi, that’s H-A-P-I or click the link in the show notes or episode page.
Barrier Macrophages
Kevin Patton (12:38):
You and I talk about macrophages a lot in A&P when we’re teaching A&P. They come up a lot. Macrophages are little scavenger cells. They’re not little, they’re big. That’s where the name macro comes from. On the cellular level, they’re pretty big cells and they do phagocytosis. And that gives us the other part of their name phage which ultimately can be translated as eating or ingesting or gobbling up. And that’s the technical terminology I like to use.
Kevin Patton (13:09):
Macrophages are the gobbling up cells. And they gobble up damaged cells and cell parts and other debris and particles that we don’t want floating around in our body. And so they have a very valuable and important role in the human body. Helping keep things clean and helping protect us from infected cells and other kinds of potentially damaging particles.
Kevin Patton (13:35):
Now, something about macrophages that I don’t really dive into much in my A&P course but you might and that is where they come from. And macrophages actually have two distinct sources of development. One cell lineage arises from monocytes. And of course, monocytes are immune cells that are derived from the bone marrow, the myeloid tissue.
Kevin Patton (13:58):
But there’s this other set of macrophages that is developing in a different way that’s independent from monocytes. In these macrophages, they come from cells that have spread out into the tissues during embryonic development. And so, those macrophages that end up in different tissues, they’re sometimes just called tissue macrophages or they might be called tissue-resident macrophages. Or a lot of times, they’re just named for whatever tissue they’re in or whatever job they’re doing in that tissue.
Kevin Patton (14:35):
And that’s an important aspect of this and that is they have different jobs to do in different tissues. And so, they’re going to express different genes depending on which subset of macrophages they are, which tissue they’re in and what job they’re doing. And so, it may be something beyond this scavenging of damaged cells and so on. Or it may be a different way of doing it or a specific set of things that they’re gobbling up. So that’s important to know about macrophages. There are different subsets of them.
Kevin Patton (15:14):
Now, when we’re looking at these tissue macrophages, we see that some of them have a role in producing an inflammatory response. But there are other subsets of macrophages that have an anti-inflammatory role. We can’t say that macrophages in general promote inflammation. And we can’t say that, in general, they inhibit inflammation. What we can say is they’re capable of either job and it just depends on which macrophage you’re talking about.
Kevin Patton (15:50):
There’s something else I want to mention before I even tell you why I’m talking about macrophages is I want to remind you of the disease rheumatoid arthritis. We need reminding of that. That’s something that is throughout our human population, we’re reminded of it frequently because a lot of people suffer from rheumatoid arthritis.
Kevin Patton (16:13):
And we’re doing a lot of work to try and relieve that suffering and produce effective treatments, and someday maybe even a cure for rheumatoid arthritis. And it’s an immune disorder that is associated with inflammation of joints. It involves also, because of that inflammation and various processes going on there with the destruction of cartilage and the destruction of bone in our joints that are affected by the rheumatoid arthritis, it turns out that macrophages have a key role in initiating rheumatoid arthritis.
Kevin Patton (16:54):
Now, in some recent research, so there it is and what you’ve been waiting for like, “Why is he talking about this now? We know all that?” Well, there’s some recent research that was looking at a specific subset of macrophages, specifically those that express a gene called CX3CR1. And I’ll never remember that. I have that written down on a little piece of paper here. CX3CR1, yeah, okay.
Kevin Patton (17:22):
But that’s a particular gene and it’s one that they were looking at. And they found that these macrophages that express that gene, they are found in the form of a layer of cells. Now, that’s weird, isn’t it? You always think of macrophages as being these somewhat independent scavengers. They’re like cats roaming around independently of each other and gobbling up mice.
Kevin Patton (17:49):
But these CX3CR1 … I hope I don’t lose this paper. I hope it doesn’t drop on the floor, CX3CR1 expressing macrophages. They are found as a layer of cells. And that layer of cells forms a barrier like this very thin protective membrane inside a healthy synovial joint. So, where they’re found in the synovial membrane is beneath that layer of synovial fluid that is being produced by the synovial membrane.
Kevin Patton (18:29):
So, the first thing you’ll hit then is this barrier made up of all these macrophages linking themselves together into a membrane. And then beyond that, you’re going to find some connective tissue with fibroblasts in there. An interesting thing about these CX3CR1 macrophages is I’m just going to call them what the researchers ended up calling them, and that is, barrier macrophages. That’s a lot easier than CX3CR1.
Kevin Patton (19:02):
Okay. Now, it’s easy for me to say. But I’ve said it a bunch of times. But I’m still going to call them barrier macrophages. So the barrier macrophages, it turns out when they looked at them very closely in terms of what genes were they expressing besides the CX3CR1 is that they were expressing genes for proteins that are associated with producing tight junctions in epithelial cells that are connecting together to form a membrane.
Kevin Patton (19:31):
I mean, we all know about tight junctions and what they do. And they form a seal between the adjacent epithelial cells. So, why would macrophages be making the proteins needed for tight junctions? Well, maybe it’s so that they can form this layer, this barrier that is on the surface of the synovial membrane adhering to the connective tissue and facing into the synovial fluid. So, that’s weird and interesting.
Kevin Patton (20:04):
And when they looked at this barrier layer, this layer of barrier macrophages, they found that it was really … well, the term they used is dynamic. It was not just sitting there, it was reacting to things. So, in a set of experiments, they induced arthritis in their experimental animals. And when that happened, when they induced arthritis, that barrier layer started remodeling itself. It loosens the interactions between them and those fibroblasts on the inside so that it started peeling away a little bit.
Kevin Patton (20:45):
Something that happened there is that they started ingesting, gobbling up and removing some of the inflammatory immune cells specifically the neutrophils, that they come in and they accumulate in an inflamed area and then they die. And that happens in arthritis when there’s inflammation. They get in there and these macrophages gobble them up.
Kevin Patton (21:16):
And then, they had some animals … they used mice, they’re lab mice. They induced arthritis in a group of these mice. They did that while also messing with that layer of barrier macrophages. So, they caused the arthritis and they messed up the barrier. And what happened was that those animals got much more severe arthritis than the ones where they didn’t mess with the barrier.
Kevin Patton (21:47):
So when they didn’t mess with the barrier, the barrier peeled back and started gobbling up the neutrophils. But the ones where they messed with that barrier, those barrier macrophages, then the mice got worse arthritis than otherwise. So, whatever was going on there with those barrier macrophages got messed up and the animals suffered worse from the arthritis.
Kevin Patton (22:11):
What they’re thinking now is what’s going on there? I mean, this is a new discovery. We never saw that before. That’s really interesting. And maybe here is a pathway to finding some better treatments for rheumatoid arthritis or other inflammatory conditions. Let’s find out what exactly is going on there. Let’s see what is going on during this dynamic process of reducing the effects of inflammation in arthritis.
Kevin Patton (22:43):
There’s a little bit something different that I never knew about synovial membrane. None of us knew it before. And I’m not saying we need to go into that much detail when we’re talking about synovial membranes or mentioning arthritis in our course. But it’s another one of those things that we can just drop in there and say, “This is still an active area of research.”
Kevin Patton (23:01):
We don’t know everything there is to know about how these membranes of the body are built and how they function and how they interact with other kinds of tissues that may be discussed outside of our usual discussion of joints and membranes.”
Sponsored by HAPS
Kevin Patton (23:19):
Marketing support for this podcast is provided by HAPS, the Human Anatomy and Physiology Society, promoting excellence in the teaching of human anatomy and physiology for over 30 years. Looking for teaching tips and articles outlining research about what works in teaching and learning anatomy and physiology? Well, you need to check out the HAPS Educator available online at theAPprofessor.org/haps. That’s H-A-P-S.
Interstitium
Kevin Patton (23:56):
Did you see or hear any of those headlines last week that a new organ was discovered in the human body? It’s called the interstitium. And it’s made up of little fluid spaces in the connective tissues in the wall of hollow organs like the submucosa. And it’s found in the fascia of muscles and in the skin and in lots of other places in the body.
Kevin Patton (24:17):
And I don’t know if you’re thinking, “Well, I’m thinking about these, but don’t we already know that there’s an interstitium? Don’t we already know that interstitial fluid forms little pockets within some of the connective tissues of the submucosa and other areas of the body? And not only that, even if we had not known that before, would discovering them and identify them, would it constitute an organ? Really? Isn’t it a part of an organ, really a structure within a tissue that makes up an organ?”
Kevin Patton (24:50):
I’m not the only one that has had that reaction, it turns out. A lot of scientists are pushing back and saying, “Wait a minute. This is not new information.” At least not in the way that it’s being portrayed in the headlines and even by the authors, that this is a new organ discovered in the human body. That’s taking it way beyond what they’re really seeing here.
Kevin Patton (25:16):
We’ve seen those pools of interstitial fluid for a long time. We know that interstitial fluid forms these little pockets. We know that eventually it drains into the lymphatic system, into the lymphatic capillaries and makes its way back to the bloodstream eventually.
Kevin Patton (25:34):
You know what’s new here? Well, they did some interesting visualizations. They used a kind of microscopy called endomicroscopy where they take an endoscope and used that as a microscope. And they can make images down to a depth of about 60 or 70 microns beyond the surface that the endoscope is at. And so they did that and some other interesting imaging techniques and so on. And pointed out that when we’re looking at histology slides in our course for example or in a textbook; the collagen bundles look denser than they would in life because these pools drain out and collapse.
Kevin Patton (26:18):
And, of course, we’ve known that for a long time. But it is I think important to go back and really think about all of those little fluid spaces being there and the function that they might have. There is a growing awareness of all the different kinds of mechanical and chemical and even electrical interactions in extracellular matrix and tissues throughout the body.
Kevin Patton (26:44):
And I think that this article contributes to that overall conversation that we’re having and increasing awareness of the dynamic nature of these tissues which not all that long ago were thought of to be more or less glue or packing material or reinforcement material in the body, and not really an active dynamic area that is involved in so many different functions. It’s important for homeostatic balance in our body.
Kevin Patton (27:13):
So, I do have the link to this article. It’s an open access article. I have a link to it in the show notes and on the episode page at theAPprofessor.org. I also have a diagram at the episode page. And I also have some other articles including an article that rebuts the premise that this is a new discovery and that it’s even an organ.
Button and Zipper Junctions
Kevin Patton (27:48):
Don’t you just love those moments in our career teaching A&P where we run across some information that’s been out there for a little while that seems pretty basic and pretty important to our understanding of human structure and function and we somehow missed it? I don’t know about you but I ‘m thinking, “Oh, my gosh, everybody else knows this but it just went right past me and I didn’t even see it and now I’m seeing it. And how could I not have known that? And I wish I had known this a long time ago.”
Kevin Patton (28:17):
And I just ran across some information like that, but we all have those kinds of moments. Because how can anyone possibly keep up with this huge explosion of knowledge about human biology? There’s just too much out there to keep up with. So, we do the best we can. And so, I don’t feel bad about this. I feel excited about the fact that I’ve made this discovery. And maybe you already know this, maybe you don’t, but I’m going to share it with you because I think it’s fun.
Kevin Patton (28:43):
And that is the idea that there are junctions in between the endothelial cells that make up the wall of the lymphatic capillaries that are a little bit different than I ever imagined them. And this was first proposed and demonstrated back in 2007. So it’s been out there for a while. And they’re still working on trying to iron out all the details of this.
Kevin Patton (29:12):
But we already know that the endothelial cells of the lymphatic capillaries are a little loosey-goosey. They actually overlap one another a little bit rather than being attached necessarily tightly end-to-end. And when they overlap a little bit, they form little microscopic valves that allows fluid from the tissues to push into the lumen of the lymphatic capillary. And then it becomes lymph and it travels the rest of the way through the lymphatic system and eventually is returned to the blood supply. That part we already knew.
Kevin Patton (29:50):
What I didn’t know is that in 2007, we outlined the idea that there are certain types of junctions that allow that to occur. And they’re called button junctions and zipper junctions. And they’re actually called that. I mean, can you believe that somebody didn’t get out their Latin and Greek dictionaries and try to put together a multi-syllable word for these junctions? But they didn’t because the button junctions, they’re like buttons. And these are the kind of junctions we would typically see in the adult lymphatic capillaries.
Kevin Patton (30:22):
The way they work is just like the button on our shirt. So, imagine or maybe you don’t have to imagine that you’re wearing a shirt right now that is buttoned up the front. And imagine that the left side of your shirt and the right side of your shirt are adjacent endothelial cells that are forming the wall of the lymphatic capillary. And they overlap a little bit just like they would in the lymphatic capillary.
Kevin Patton (30:47):
But they can’t be totally loose because they would just fall apart. They have to be held together at some point. And they are, they’re held together by buttons. But think about the gaps between the buttons. Right now, try to slide a finger or two or maybe part of your hand in between two of the buttons on your shirt. And you can do that very easily.
Kevin Patton (31:07):
So, imagine that that is fluid that is traveling from the interstitial space of the tissue, that’s tissue fluid, that is traveling into the lumen of the lymphatic capillary and now it’s becoming lymphatic fluid. And that’s how it works. So that that little flap there that has formed between the buttons, that’s your lymphatic capillary valve that is allowing the fluid to come into the lumen of the lymphatic capillary in this case.
Kevin Patton (31:37):
And there are junctions just like those buttons made up of various proteins. And they’re still working out how they’re built and what they’re made of and so on. But they’re the same kinds of materials that you would find with other cellular junctions, but this is a unique kind of cellular junction.
Kevin Patton (31:54):
Now, what about zipper junctions? Those are junctions that the evidence so far indicates occur only during embryonic development. It seems that our lymphatic capillaries are mostly zipped up during embryonic development, at least certain stages of embryonic development. And then they eventually unzip or the zippers sort of dissolve and they’re sort of reconstituted. We would call this a case of plasticity where the cell is changing things around and changing the connections from buttons to a zipper.
Kevin Patton (32:28):
Now, think about how a zipper is built. Those connections between the two sides of the zipper, they’re made up of all kinds of little tiny elements that hook together. So, therefore, it is a much more continuous junction compared to when we have buttons.
Kevin Patton (32:45):
So, imagine you have a shirt or a jacket or something that is zippered up the front instead of having buttons. Now, you can’t easily slip your finger or much of anything in between those two sides of your garment like you could with the buttoned-up garment. And so that’s preventing things from getting through.
Kevin Patton (33:04):
So, it’s important that embryologically, we go through that step of changing from the zippered form to the buttoned form. And the reason I ran across it recently was because there was a new study from some researchers at Yale that accidentally, they were trying to produce some laboratory mice that were obese so they could do some studies on it.
Kevin Patton (33:26):
And what they did was they accidentally produced some mice whose lacteals, the lymphatic capillaries in the intestinal villi, were zipped up instead of having buttons. So that meant that the chylomicrons that should have been absorbed from the gut and into the lymphatic pathway weren’t being absorbed. And so, instead of ending up with obese mice, they ended up with mice that could not become obese because they weren’t absorbing fats that were in their diet. So they were giving them more and more fat in their diet and they just weren’t getting fat.
Kevin Patton (33:59):
And then they figured out what was going on. So, they’re thinking knowing about this might help control the condition in people who are already obese and maybe we can sort of shut down their absorption of fats for at least a little while until they’re in a healthier range.
Kevin Patton (34:16):
I think I ‘m going to do this as a demonstration in my class from now on. I’m going to demonstrate using a shirt. Maybe I can take a shirt and a zippered garment and put them on the torso model from the lab and demonstrate that. Actually, the students themselves can do that if they have a buttoned or zippered garment on in class. And they can do that themselves and understand how the lymphatic capillaries work, including the lacteals.
Kevin Patton (34:42):
And you might want to bring up this new information if you want. It might be a good opportunity to stimulate some critical thinking like, “Okay, let’s say we come up with a drug that can convert or maybe some kind of gene therapy or something that can convert the button form to the zipper form of connection in the lacteals. Would that really reduce a person’s weight?”
Kevin Patton (35:03):
Well, let’s say it does but what other consequences might that have? Could there be some unwanted side effects in that case? I think there probably could. That’s not a done deal yet. And so that gets them thinking, not only thinking critically, but thinking scientifically which is a form of critical thinking. There you go, something new I learned. Maybe it’s new for you, too.
Lymphatic Micro-Organ
Kevin Patton (35:28):
A couple of weeks ago, I ran across a headline that stated, “Researchers Discover New Micro-Organ in Human Immune System.” And you know me, I’m always attracted to headlines that claim that there’s a new organ in the human body because, well, sometimes there is. And what really intrigued me about this one is they didn’t really call it an organ, they called it a micro-organ. And I don’t even know what that is so I had to read the article.
Kevin Patton (35:56):
And I’m glad I did because it was referring to a piece that came out on August 22nd in Nature Communications. And it’s entitled Memory B-cells are Reactivated in Subcapsular Proliferative Foci of Lymph Nodes. And basically what it described was some experiments in which they demonstrated that memory B-cells that are produced during and after an infection in an area get trapped in the nearby lymph nodes which is not surprising. And they hang out there which is also not surprising.
Kevin Patton (36:39):
But they form a focus, a location that is distinct from the germinal center of the lymph node. It’s distinct both functionally and structurally from the germinal center. And these folks decided to call it a subcapsular proliferative focus or plural would be foci or foci. It’s subcapsular because it’s just inside the capsule, just deep to the capsule which forms the wall of the lymph node.
Kevin Patton (37:14):
And it’s proliferative because it’s made up of memory B-cells which we know when triggered will proliferate and form groups of more memory B-cells and some plasma cells which are going to be actively producing antibodies against the antigen that triggered the formation of those memory B-cells to begin with.
Kevin Patton (37:39):
It’s called a focus because it’s a location. These SPFs which is a lot easier to say than subcapsular proliferative foci or foci, so the SPFs, that’s what new. And the authors, I couldn’t find anywhere in there where they called it a micro-organ, maybe I just missed it. But the point is is that we’ve never really seen it before or never really noticed it before.
Kevin Patton (38:08):
And it’s really interesting that when these memory B-cells, they hang out there, which makes sense they’d hang out in the lymph node but at a particular location just inside the capsule where they are most likely to encounter the antigen that they’re programmed for would be right there in the outer area, not deep in the germinal center. So it makes sense that it would be there.
Kevin Patton (38:35):
And it also makes sure that it’s a good place for the macrophages which are acting as antigen-presenting cells that they would be able to get to those memory B-cells very easily. And not only are the memory B-cells hanging out there but there are a bunch of helper T-cells and presumably other cells that are going to be involved in this whole process of getting those memory B-cells activated and proliferating and producing the plasma cells which are going to be producing the antibodies.
Kevin Patton (39:11):
And all of this together means that that process of this secondary response to the antigen, the original antigen, is going to be that much more efficient. And now, we’re seeing how it gets to be so efficient. And the authors of this communication proposed that knowing about this may help us do vaccines better because isn’t that what vaccines are doing is giving us that original antigen exposure and getting those memory B-cells in place.
Kevin Patton (39:43):
Now, we know where there place is, at least one of the places is, that they’re going to be ready at a moment’s notice to mount that very strong and very rapid secondary response which is the whole point of doing a vaccine, some interesting things in the immune system these days.
Free Update Newsletter from The A&P Professor
Kevin Patton (40:06):
I have more discoveries in human anatomy to discuss. But before I do, I want to mention something called The A&P Professor Science and Education Updates Newsletter. It’s a free digital subscription that you can get by going to theAPprofessor.org/updates. And it includes well, as the name implies headlines from all over the world having to do with human science of interest to faculty who teach anatomy and physiology.
Kevin Patton (40:37):
And there are also education updates with teaching and learning ideas and concepts and news from the world of education. And there are a few updates from the world of The A&P Professor. So, if you want to subscribe to that or even just check out what some of the past issues look like, go to theAPprofessor.org/updates.
New Vessels in Bone
Kevin Patton (41:05):
I was reading through some articles from new scientist and I got to tell you, when I see an article that begins with the statement, “It’s time to rewrite the anatomy books,” I’m going to read that article. And I’m glad I read this one because there’s a very interesting new discovery about a potential new kind of blood vessel that’s been discovered in bones. Whether it’s really going to require a rewrite of anatomy books is yet to be seen, but this is very interesting early information that you probably ought to take a look at because I think there is something to it.
Kevin Patton (41:41):
You probably already know that the blood supply of bones usually comes into the bone by way of some arteries at either end of a long bone or maybe near the middle of a long bone. And it penetrates through the cortical layers of bone all the way down to the medullary cavity. And then from there, it radiates back to the outer areas of the bone.
Kevin Patton (42:12):
And what these researchers that wrote a recent article in Nature Metabolism did was they were looking in mice. And they saw that by using some chemicals on some long bones of a mouse, they were able to make the bone transparent. And they could see the tiny little capillaries that were present in the bone. And they found a bunch that they did not expect that were crossing the bone shaft perpendicularly.
Kevin Patton (42:45):
In other words, they were going right across those cortical layers and right down toward the medullary cavity. So they weren’t coming in in a larger artery and then going through this whole network of capillaries and so on within the bone and then draining back out through a large vein or maybe two or three or whatever large veins out of that long bone.
Kevin Patton (43:07):
They were actually coming in, sort of seeping in, through the wall of the bone. But, of course, they’re going through these little capillaries. And the same thing for blood escaping back from inside the bone and getting back into the venous circulation back toward the heart. And so, they named these newly discovered, very tiny vessels, transcortical vessels or TCV.
Kevin Patton (43:36):
And then, of course, one of the first things they did, which I would do, is look in human bone and see, and they did find some in human bones. But there’s a lot more yet to be done with not only the mouse model but also in doing human investigation to see whether this is just a fluke or it’s a mistake in how they were applying the technology or a mistake in how they recorded their observations or what. But it’s looking pretty good so far.
Kevin Patton (44:00):
And by the way, in the journal article, they proposed that over 80% of the arterial blood flow coming into the bone and about 59% of the venous blood flowing out of the bone goes through these TCVs and not through those large arteries and veins that we thought were the only way in and out of a bone. So, this could really be a boon for medical illustrators who are going to have to draw new pictures of the blood supply of bones. And I think it’s just another one of those interesting stories on our journey to understanding the anatomy of the human body.
Tubarial Salivary Glands
Kevin Patton (44:44):
Can you believe it? Yet another previously undiscovered new organ has been discovered in the human body. And this time, it’s the tubarial salivary gland which its discoverers would like to see considered to be one of the major salivary organs along with the parotid, submaxillary and submandibular pairs, rather than this simply another set of the huge number of minor salivary glands that are scattered all around the mouth and throat regions.
Kevin Patton (45:23):
The name tubarial comes from its location or I mean their location because it is a paired set. So, the location is along the torus tubarius. And, yeah, I wasn’t sure what that is either when I first heard it. A torus is basically a classic donut shape. And that’s kind of the shape formed by the cartilage supporting the opening of the auditory tube into the nasopharynx.
Kevin Patton (45:54):
The pharyngeal mucosa then has these rounded bumps surrounding the tubes’ opening, looking like there’s a little doughnut under it. That is what the torus tubarius is. So, yeah, okay, we’re a miniaturized in the nasopharynx, looking directly at the opening of the auditory tube. And embedded in that tubarial mucosa and extending inferiorly from there are a whole bunch of exocrine glands producing a mucus secretion that’s coming out of a whole bunch of little ducts.
Kevin Patton (46:31):
The image in the show notes in your podcast app or at the episode page shows this structure clearly if you can’t imagine it. That image looks almost as if somebody had been miniaturized and took a snapshot with their mobile phone. And mark my word, someday that’s going to be a thing.
Kevin Patton (46:52):
Now, I’m always skeptical of discoveries of new major organs, so I’m still taking a wait and see attitude, at least a little bit. Yes, the discoverers did look at many, many individuals and made all kinds of other observations that back up their claim, to a point. But I’m thinking maybe we need a little bit more. I’m not sure. And, of course, we need time for science to do its job and let folks replicate and debate and mull over what’s going on.
Kevin Patton (47:28):
A question I have is that there are multiple ducts observed in the tubarial salivary gland. And I’m not sure, therefore, how it can be distinguished from groupings of the many minor salivary glands we’ve already established in anatomy. On the other hand, the sublingual salivary glands have multiple ducts, so I guess the fact that there’s a bunch of ducts doesn’t exactly push the tubarial salivary glands off the list.
Kevin Patton (48:04):
Any list of what’s an organ and what’s not an organ or what’s a major organ and what’s not a major organ and it’s a minor organ is only partly a matter of science theory. It’s also partly a matter of our need to figure out what label we want to put on structures. Those labels are there to help us understand the body better and also to communicate more accurately with each other.
Kevin Patton (48:35):
So what the community of scientists needs to do now is to figure out whether this newly proposed name and newly proposed designation is a major salivary gland rather than a minor salivary gland is useful or not. Now, I don’t have a real strong opinion one way or the other about this, just questions.
Kevin Patton (48:59):
A big question is, why insist on calling it an organ? In reading the paper, you’ll see that the author’s primary interest in doing so has to do with the clinical implications. If it’s one of the major salivary glands, then it’s worth putting on the list of structures that we want to take steps to spare or protect during radiation therapy. And that’s where these folks are coming from, from the radiation therapy angle.
Kevin Patton (49:33):
If the tubarial salivary gland is just a random set of tiny glands we imagined to be scattered all over the place, well, then maybe sparing them is impractical. But I think the authors are saying, “Hey, look at these images. These glands are concentrated in a rather defined area. And there are a lot of them. And we can take steps to avoid damaging them now that we know where they are and that they’re even there. And patients will be better off for doing that.
Kevin Patton (50:11):
So here they are and here’s what we’re calling them because they need a name to put on our list of things to consider when planning radiotherapy for a patient.” So, when you look at it from that angle, maybe calling this structure an organ is not such a bad idea. I don’t know.
Kevin Patton (50:32):
As usual, some folks are calling for a rewriting of textbooks. Well, I always want to hold on a minute when I hear that because I hear that a lot. Maybe my ears are sensitized to that. What? Something needs to go into a textbook? And a lot of times, it’s something that’s just way too early to go into a textbook, something that’s going to be soon disproven or at least modified in some way.
Kevin Patton (50:57):
And the other thing is is that especially for undergraduate A&P textbooks, we have to ask the question, “Is this really a detail that our students really need to know?” Even at an advanced level like in a medical anatomy course, there are some things that maybe are just too much and maybe don’t have a clinical or practical application.
Kevin Patton (51:19):
I think this one does but I’m just saying, in general, those are some questions that have to be asked before it actually gets into textbooks. Things don’t just automatically flow from journals into a textbook. There’s all kinds of editorial decisions to be made and scientific questions and decisions and observations need to be made.
Kevin Patton (51:38):
So, are we really ready for that at this moment? I don’t know. Maybe science has to do its work a little bit more so that we have greater confidence in this idea. Or maybe it is time now. But no matter what, I’m also thinking it’s a great time to mention it to our students. Even if it’s outside the official content of our course, that is, maybe even if we’re not going to put it on the test, make it into a test item, maybe we want to discuss how science works. And this is a good opportunity to do that.
Kevin Patton (52:15):
And it’s also a good opportunity to discuss that we don’t already know everything. And it’s a good opportunity to discuss what makes an organ an organ which is a lot fuzzier than a lot of students imagined. And well, there’s all kinds of interesting things that can come out of such a discussion.
Staying Connected
Kevin Patton (52:37):
Hey, why not share this episode with a colleague and get their thoughts on it? It’s easy to do. Just go to theAPprofessor.org/refer to get a personalized share link that will not only get your friend all set up. I always provide links if you want to know more about the topics of this episode. If you don’t see links in your podcast player, go to the show notes at the episode page at theAPprofessor.org/podcast.
Kevin Patton (53:10):
And while you’re there, you can claim your digital credential for listening to this episode. And you’re always encouraged to call in with your questions, your comments and ideas at the podcast hotline. That’s 1-833-LION-DEN or 1-833-546-6336. Or send a recording or written message to podcast at theAPprofessor.org.
Kevin Patton (53:39):
You’re invited to join my private A&P teaching community at theAPprofessor.org/community. I’ll see you down the road.
Aileen (53:55):
The A&P Professor is hosted by Dr. Kevin Patton, an award-winning professor and textbook author in Human Anatomy and Physiology.
Kevin Patton (54:08):
Each episode of this podcast is no deposit, no return.
This podcast is sponsored by the
Human Anatomy & Physiology Society 
This podcast is sponsored by the
Master of Science in
Human Anatomy & Physiology Instruction 
Transcripts & captions supported by
The American Association for Anatomy. 
Stay Connected
The easiest way to keep up with new episodes is, um, wherever you already listen to audio!
Click here to be notified by email when new episodes become available (make sure The A&P Professor option is checked).
Call in
Record your question or share an idea and I may use it in a future podcast!
Toll-free: 1·833·LION·DEN (1·833·546·6336)
Email: podcast@theAPprofessor.org
Share

Kevin's bestselling book!
Available in paperback
Download a digital copy
Please share with your colleagues!
Tools & Resources
TAPP Science & Education Updates (free)
TextExpander (paste snippets)
Krisp Free Noise-Cancelling App
Snagit & Camtasia (media tools)
Rev.com ($10 off transcriptions, captions)
The A&P Professor Logo Items
(Compensation may be received)
🏅 NOTE: TAPP ed badges and certificates can be claimed until the end of 2025. After that, they remain valid, but no additional credentials can be claimed. This results from the free tier of Canvas Credentials shutting down (and lowest paid tier is far, far away from a cost-effective rate for our level of usage). For more information, visit TAPP ed at theAPprofessor.org/education